Comprehensive Guidelines On Anterior Crown Preparation

The Anterior Crown is not only known for its aesthetic benefits but is also used to restore damaged tooth structures and address most occlusal issues that patients may encounter. The Anterior Crown Preparation process is considered a crucial initial step in anterior tooth restoration. Strict adherence to the guidelines for Anterior Crown Preparation is essential to maximize the optimal performance of durability, function, aesthetics, and biocompatibility of the restoration.
This article will provide you with the necessary information to ensure an effective Anterior Crown Preparation process, ultimately delivering the most optimal restorative outcomes for your patients.

The Importance Of Anterior Crown Preparation
The advantages of anterior crowns, such as strength, durability, chemical, and dimensional stability, as well as biocompatibility, can be maximized if the Anterior Crown Preparation process is carried out effectively.
Additionally, since anterior crowns are placed in highly aesthetic zones, both functionality and aesthetics must be ensured. This can be achieved through the following:

- Uniform tooth reduction to enhance the durability of the restoration.
- Creating smooth margins during tooth preparation reduces stress on the crown and minimizes the risk of fractures.
- Meticulous tooth preparation to ensure the aesthetic integrity of the final restoration.
- Improving biocompatibility, chemical, and dimensional stability with advanced preparation techniques.

Guidelines For Anterior Tooth Preparation
Whether it is an anterior or posterior crown, proper dimensional reduction is a crucial factor in the Anterior Crown Preparation process. Different crown materials require specific preparation techniques. Therefore, it is essential to follow the guidelines and adhere to precise measurements to ensure appropriate circumferential and incisal reduction based on the selected material, facilitating clinical success.
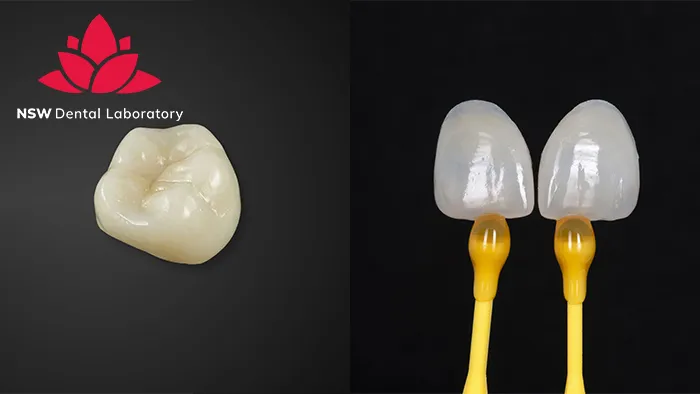
Anterior PFM Crown Preparation
To prepare an anterior tooth for a PFM (porcelain-fused-to-metal) crown, additional space must be provided to accommodate the restoration’s metal and ceramic layers. The preparation process involves several distinct steps, as detailed below:

- Clearance: The labial surface should be reduced by a minimum of 1.2 mm, ideally 1.5 mm. The lingual surfaces should be reduced by 1 mm, and the incisal edge by 2 mm to achieve optimal aesthetics.
- Retention grooves: For successful preparation of the labial surface, a central cervical groove parallel to the path of placement along the long axis of the tooth should be created. Two secondary grooves should be placed on either side. Incisal edge reduction grooves, approximately 1.8 mm deep, must extend halfway down the labial surface.
- Circumferential chamfer: Proximal contacts are reduced, and a 0.5-mm lingual chamfer is created. The incisal edge should be reduced by approximately 2 mm to allow sufficient space for the ceramist to create a crown with adequate material thickness and good incisal translucency.
Besides that, use a football-shaped diamond bur to contour the lingual surface of the tooth. Remove the tooth structure between the depth grooves, forming a cervical shoulder approximately 1 mm wide and extending into the proximal embrasures.

Anterior Zirconia Crown Preparation
Anterior Zirconia crowns require meticulous preparation and attention to ensure they fit properly and achieve optimal aesthetics. The following measurements must be adhered to:
- Clearance: Ensure a minimum of 0.3 mm of space for crown wall thickness, with the ideal range being 1.0 mm to 1.5 mm. Maintain an incisal reduction of 1.8 mm to 2.0 mm for optimal results.
- Circumferential chamfer: The circumferential chamfer must be continuous and visible, with a minimum reduction of 0.5 mm at the gingival margin.
- Preparation angle: The horizontal and vertical preparation angles should be approximately 5 degrees and should not be beveled.
- Rounded edges: All incisal edges must be rounded, and the lingual aspect of anterior teeth should be reduced using a diamond bur to create a concave lingual surface.

Considerations For Anterior Crown Preparation
In addition to understanding the guidelines for anterior crown preparation, dentists must also consider certain factors that can render the preparation inadequate. These factors include:
- Undercuts: These can potentially “catch” on the tooth structure, compromising the fit and retention of the crown.
- Gutter preparation: A deep groove along the margin can lead to instability of the crown, increasing the risk of fractures and making cementation challenging.
- 90-degree shoulder: This can result in reduced crown stability and increased risk of breakage.
- Parallel wall preparations: These can compromise the mechanical retention of the crown.
- Sharp incisal or occlusal edges: These features can hinder proper crown placement and contribute to instability and fracture risks.
Addressing these issues during the preparation process is crucial to ensure the longevity and success of the restoration.

Support Anterior Crown Preparation with VTA Dental Lab
A meticulous Anterior Crown Preparation process is an essential part of placing a front tooth crown, and the quality of the crown itself is just as important. As one of the newest materials in dentistry, zirconia requires proper preparation steps to ensure crowns are seated successfully, delivering more beautiful smiles than ever. And beautiful smiles need a trusted dental lab partner.
By incorporating digital dentistry into nearly all workflows, we are committed to enhancing patient experiences, improving your practice’s productivity, and streamlining every aspect of your dental care delivery.

Not only for zirconia crowns and PFMs but also for a wide range of other materials, NSW Dental Lab ensures that your anterior crown preparation process, as well as restoration preparation overall, achieves the highest efficiency, maximum accuracy, and time savings.
Let NSW be your next go-to dental lab for crowns and bridges!